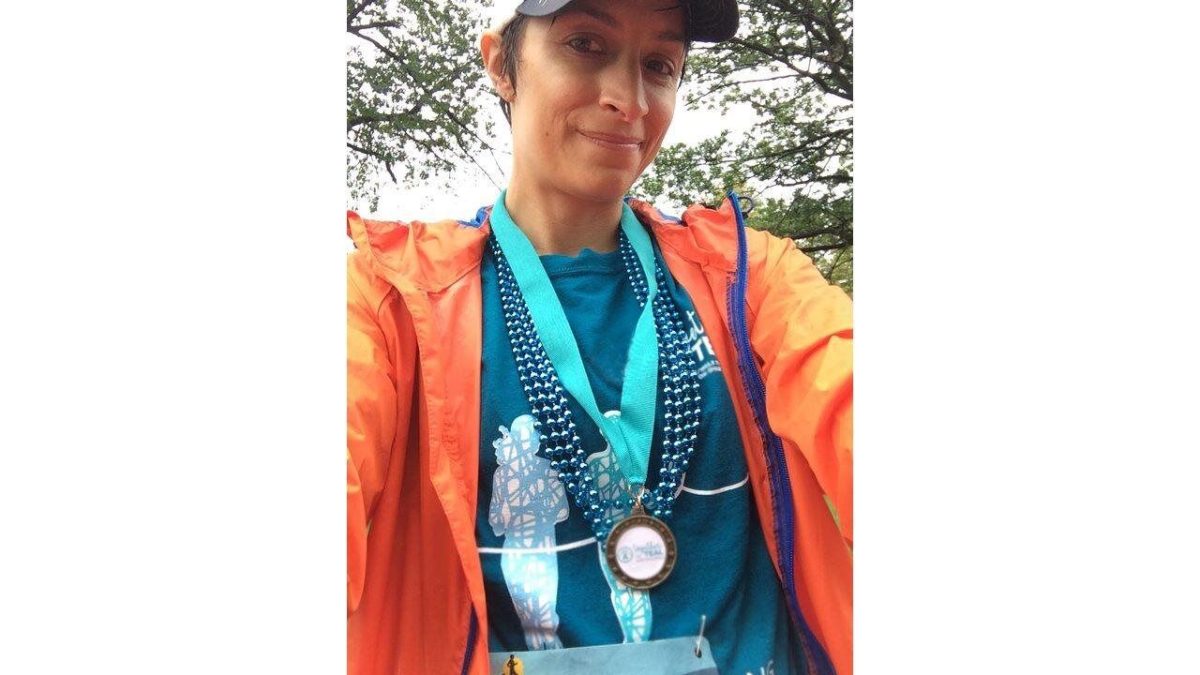
(BPT) – Richmond, Virginia, resident Tiffany Stout never realized that in the prime of her life she would not only be battling cancer, but also a cancer that is rare with limited treatment options. She quickly learned how to become an advocate for her needs and an educator to others.
Tiffany has a history of ovarian cysts, so she didn’t find it alarming when she experienced spotting and sensitivity in her abdomen. These were fairly normal symptoms for her that she thought would pass with her period as they had previously. But her symptoms persisted beyond her cycle and started to interrupt her daily life. “I noticed when I would run I would have pain in my abdomen, almost like vibrations, which made it difficult for me to exercise. I also noticed that I was retaining fluid in my love handle area. I thought I was just getting older but it was fluid from the tumor.” Frequent urination was also becoming a problem, interrupting her workday, so she reached out to her gynecologist, who urged her to follow up with her general practitioner for an ultrasound, since insurance red tape prevented her gynecologist from ordering it. When the results came back, the ultrasound revealed possibly cancerous tumors.
After a magnetic resonance imaging (MRI) test, Stout underwent surgery to remove the tumor and further testing revealed she had stage III low-grade serous ovarian cancer (LGSOC), a serious disease that often goes undiagnosed in young women like Stout.
LGSOC is serious and different
LGSOC is a rare type of ovarian cancer that disproportionately affects younger women ages 45-55, although some have been diagnosed as early as 14 years old.1 An estimated 1,000-2,000 new cases of LGSOC are diagnosed every year in the U.S.2 LGSOC represents 6-8% of all ovarian cancers.1
Despite being classified as a separate disease in 2014, more recognition is needed around the differences between the more common high-grade serous ovarian cancer (HGSOC) and LGSOC so that it can be diagnosed and treated sooner.3
LGSOC is difficult to diagnose, as symptoms — such as back or pelvic pain, feeling full quickly, constipation or other changes in bowel habits — can often be overlooked as not being related to cancer.4,5,6 This is particularly the case when doctors examine younger women as ovarian cancer is generally thought to be uncommon at their age.1 For these reasons, LGSOC is likely to be diagnosed when it has already spread outside of the ovaries.7 Yet for many, LGSOC and its treatment will have a long-lasting impact on mental and physical health, including fertility and early menopause.8,9,10
Stout’s journey to treatment
Stout’s diagnosis in her 30s was especially troubling because there was little understanding and information about LGSOC as its own disease, subsequently leaving many tough decisions in her court to make. “My doctor said it was low-grade and my treatment options would be impacted, but when I went to do my own follow-up research to make an informed choice about my treatment, there was not anything low-grade specific I could find. It all spoke to the more common HGSOC.”
Unfortunately, once diagnosed with LGSOC, there are limited treatment options available and these are based on other cancer treatment strategies.11 While the standard of care for ovarian cancer is chemotherapy, LGSOC is chemotherapy-resistant, meaning chemotherapy stops working for nearly all women with LGSOC.1,11
“I still had to go through chemotherapy to qualify for any clinical trials — a process that was difficult to navigate alone,” said Stout. “Even then, it took multiple medical opinions to finally get a management plan for my condition. I needed to remain constantly on top of my doctors and learned how to become an advocate for myself.”
Even with treatment, LGSOC is highly recurrent.12 About 85% of people who achieve full remission following first-line treatment will have their cancer come back.12 But there is hope on the horizon with promising treatment options being investigated to see if they can work for people living with LGSOC.
Awareness and patient advocacy
The LGSOC community has been working hard to raise awareness of the disease, advance research and provide resources that help educate and connect patients — but there is still room to build upon existing efforts.
“It can be challenging to balance hunting down information while also living your life, so it’s important for people to have better access to key information about LGSOC so they can make informed decisions about their management plan in partnership with their doctor,” said Stout. “I also wish that there were more tools that helped connect patients to support groups as it can often feel very isolating living with a rare disease like LGSOC.”
“Since LGSOC is a relatively newly recognized form of cancer, it is unfortunately not unusual that many doctors have never diagnosed a LGSOC case before and could be seeing it for the first time in their patients,” says Dr. Jubilee Brown of the Levine Cancer Institute. “This makes it especially important that women have resources available specifically for LGSOC and are encouraged to talk about their unique experiences with their doctor so they can figure out the best path forward together.”
If you or a loved one may be experiencing symptoms or want to learn more, visit LetsTalkAboutLGSOC.com for helpful resources and information on LGSOC.
[1] Grisham, R. Low Grade Serous Carcinoma of the Ovary. Oncology. 2016. 30(7):650-652. Available at: https://www.cancernetwork.com/view/low-grade-serous-carcinoma-ovary. Accessed March 2023.
Tiffany has a history of ovarian cysts, so she didn’t find it alarming when she experienced spotting and sensitivity in her abdomen. These were fairly normal symptoms for her that she thought would pass with her period as they had previously. But her symptoms persisted beyond her cycle and started to interrupt her daily life. “I noticed when I would run I would have pain in my abdomen, almost like vibrations, which made it difficult for me to exercise. I also noticed that I was retaining fluid in my love handle area. I thought I was just getting older but it was fluid from the tumor.” Frequent urination was also becoming a problem, interrupting her workday, so she reached out to her gynecologist, who urged her to follow up with her general practitioner for an ultrasound, since insurance red tape prevented her gynecologist from ordering it. When the results came back, the ultrasound revealed possibly cancerous tumors.
After a magnetic resonance imaging (MRI) test, Stout underwent surgery to remove the tumor and further testing revealed she had stage III low-grade serous ovarian cancer (LGSOC), a serious disease that often goes undiagnosed in young women like Stout.
LGSOC is serious and different
LGSOC is a rare type of ovarian cancer that disproportionately affects younger women ages 45-55, although some have been diagnosed as early as 14 years old.1 An estimated 1,000-2,000 new cases of LGSOC are diagnosed every year in the U.S.2 LGSOC represents 6-8% of all ovarian cancers.1
Despite being classified as a separate disease in 2014, more recognition is needed around the differences between the more common high-grade serous ovarian cancer (HGSOC) and LGSOC so that it can be diagnosed and treated sooner.3
LGSOC is difficult to diagnose, as symptoms — such as back or pelvic pain, feeling full quickly, constipation or other changes in bowel habits — can often be overlooked as not being related to cancer.4,5,6 This is particularly the case when doctors examine younger women as ovarian cancer is generally thought to be uncommon at their age.1 For these reasons, LGSOC is likely to be diagnosed when it has already spread outside of the ovaries.7 Yet for many, LGSOC and its treatment will have a long-lasting impact on mental and physical health, including fertility and early menopause.8,9,10
Stout’s journey to treatment
Stout’s diagnosis in her 30s was especially troubling because there was little understanding and information about LGSOC as its own disease, subsequently leaving many tough decisions in her court to make. “My doctor said it was low-grade and my treatment options would be impacted, but when I went to do my own follow-up research to make an informed choice about my treatment, there was not anything low-grade specific I could find. It all spoke to the more common HGSOC.”
Unfortunately, once diagnosed with LGSOC, there are limited treatment options available and these are based on other cancer treatment strategies.11 While the standard of care for ovarian cancer is chemotherapy, LGSOC is chemotherapy-resistant, meaning chemotherapy stops working for nearly all women with LGSOC.1,11
“I still had to go through chemotherapy to qualify for any clinical trials — a process that was difficult to navigate alone,” said Stout. “Even then, it took multiple medical opinions to finally get a management plan for my condition. I needed to remain constantly on top of my doctors and learned how to become an advocate for myself.”
Even with treatment, LGSOC is highly recurrent.12 About 85% of people who achieve full remission following first-line treatment will have their cancer come back.12 But there is hope on the horizon with promising treatment options being investigated to see if they can work for people living with LGSOC.
Awareness and patient advocacy
The LGSOC community has been working hard to raise awareness of the disease, advance research and provide resources that help educate and connect patients — but there is still room to build upon existing efforts.
“It can be challenging to balance hunting down information while also living your life, so it’s important for people to have better access to key information about LGSOC so they can make informed decisions about their management plan in partnership with their doctor,” said Stout. “I also wish that there were more tools that helped connect patients to support groups as it can often feel very isolating living with a rare disease like LGSOC.”
“Since LGSOC is a relatively newly recognized form of cancer, it is unfortunately not unusual that many doctors have never diagnosed a LGSOC case before and could be seeing it for the first time in their patients,” says Dr. Jubilee Brown of the Levine Cancer Institute. “This makes it especially important that women have resources available specifically for LGSOC and are encouraged to talk about their unique experiences with their doctor so they can figure out the best path forward together.”
If you or a loved one may be experiencing symptoms or want to learn more, visit LetsTalkAboutLGSOC.com for helpful resources and information on LGSOC.
[1] Grisham, R. Low Grade Serous Carcinoma of the Ovary. Oncology. 2016. 30(7):650-652. Available at: https://www.cancernetwork.com/view/low-grade-serous-carcinoma-ovary. Accessed March 2023.
[2] Verastem Data on File.
[3] Kurman RJ, Carcangiu ML, Herrington CS, Young RH, editors. WHO Classification of Tumors of Female Reproductive Organs, 4th ed; 2014.
[4] About Low Grade Serous Ovarian Cancer. Cure Our Ovarian Cancer. https://cureourovariancancer.org/us/about/low-grade-serous-ovarian-cancer/. Accessed March 2023.
[5] Understanding Low-Grade Ovarian Cancer and Its Effects. Healthline. https://www.healthline.com/health/ovarian-cancer/low-grade-ovarian-cancer. Accessed March 2023.
[6] Ovarian Cancer Symptoms. Cure Our Ovarian Cancer. https://cureourovariancancer.org/us/ovarian-cancer-symptoms/. Accessed March 2023.
[7] Findlay et al. The Ovary (Third Edition). 2019. Pages 1-3.
[8] Key Statistics for Ovarian Cancer. American Cancer Society. https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics. Accessed March 2023.
[9] Norton, Tina R. Ovarian Cancer Patients’ Psychological Distress: The Role of Physical Impairment, Perceived Unsupportive Family and Friend Behaviors, Perceived Control, and Self-Esteem. APA PsycNet. https://psycnet.apa.org/record/2005-02260-003. Accessed March 2023.
[10] Social & Emotional Impacts of Cancer. MD Anderson Cancer Center. https://www.mdanderson.org/patients-family/life-after-cancer/social-emotional-impacts.html. Accessed March 2023.
[11] Ovarian Cancer Guidelines 2022. National Comprehensive Cancer Network. https://jnccn.org/view/journals/jnccn/20/9/article-p972.xml?ArticleBodyColorStyles=inline%20pdf. Accessed March 2023.
[12] Corrado G, Salutari V, Palluzzi E, Distefano MG, Scambia G, Ferrandina G. Optimizing Treatment in Recurrent Epithelial Ovarian Cancer. Expert Rev Anticancer Ther. 2017; 17:1147-1158. doi: 10.1080/14737140.2017.1398088.